
Dry Eye Syndrome, frequently just called ‘dry eyes,’ affects millions each year, yet it’s often trivialized as minor irritation. It’s a chronic condition where the eyes don’t produce enough volume of tears or the right quality of tears to stay adequately lubricated.
This lack of lubrication can lead to more than just a fleeting sense of discomfort. It can significantly diminish someone’s quality of life, making everyday activities like reading, using a computer, or driving particularly challenging.
A common misconception about dry eyes is that it’s simply a sign of aging or a temporary side effect of a windy day. While these factors can play a role, the condition is multifaceted with a range of causes including medical conditions, medications, and environmental factors.
Detecting DES goes beyond noticing the occasional itchiness or redness. Symptoms can include stinging or burning sensations, a feeling of something in your eye, episodes of excess tears following very dry eye periods, and a mucus discharge from the eye.
What is Ocular Surface Staining?
If you experience dry, scratchy, or irritated eyes, your eye doctor might use a technique called ocular surface staining to get a closer look at the possible causes. But what exactly is this process, and what does it tell us about your eye health? Ocular surface staining is a diagnostic tool that allows eye care professionals to visualize damage or disease on the surface of your eye. By applying a special dye, such as fluorescein or lissamine green, to the ocular surface, they can identify problems that are often invisible to the naked eye.
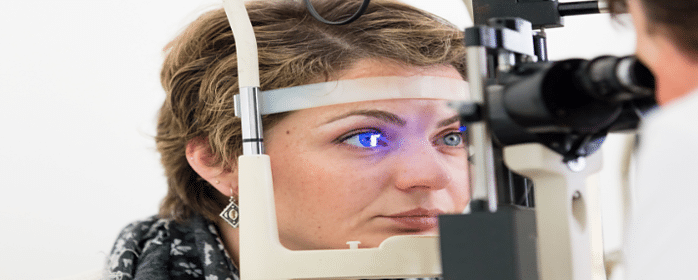
When it comes to Dry Eye Syndrome or DES, ocular surface staining is particularly revealing. DES damages the tear film that protects the cornea, leading to dry spots that can become inflamed or even scarred in severe cases. During the examination, the dye used in ocular surface staining adheres to these dry areas and damaged cells, making them stand out under a special blue light. This not only confirms the presence of DES but can also help gauge its severity.

The process itself is simple and usually painless. Your doctor will apply the dye. Then, using a slit-lamp microscope, which shines a blue light into the eye, they will look for patterns of staining. The patterns tell a story about your eye health: punctate stains may indicate mild irritation, while more widespread staining could suggest a more serious condition.
Knowing what to look for is crucial. Corneal staining must be interpreted by a trained professional, as it can also indicate other conditions aside from DES, such as infection or abrasions. By understanding the stain patterns, your doctor can create a targeted treatment plan to relieve your symptoms and protect your vision.
With an accurate diagnosis in hand, we can turn toward effective management strategies. These strategies aren’t just about reacting to discomfort but preventing further harm and improving your overall eye health. I’ll go over some of these treatments next, explaining how they work and how they can help you alleviate the dryness and irritation associated with Dry Eye Syndrome.
Modern Management of Dry Eye Syndrome
Dry Eye Syndrome (DES), a condition that affects millions worldwide, requires attention not only because of the discomfort it causes but also due to its potential to inflict long-term harm to your vision. When I mention treatment options, you might think it’s all about eye drops. However, it’s a multifaceted approach that can truly make a difference.
Consider eye drops the first line of defense. They range from over-the-counter artificial tears to prescription anti-inflammatory drops. But the conversation doesn’t end there. For some, lifestyle changes such as avoiding blast of air from fans or air-conditioners, using a humidifier, or incorporating omega-3 fatty acids into their diet can be just as essential.
When conventional methods don’t suffice, medical procedures bring hope. Small devices called punctal plugs can be inserted to block tear drainage, thereby retaining moisture. In more severe cases, surgeries that permanently close the tear ducts may be recommended.
Some people might overlook the significance of a timely diagnosis, but it’s crucial. Putting off a visit to your eye care professional could lead to more severe DES. Early intervention is key to keeping those eyes healthy.
Technological advances are revolutionizing the treatment landscape. Imagine contact lenses that release moisture throughout the day or cutting-edge imaging technology that monitors the health of the ocular surface. These developments are changing lives, offering newfound comfort to those previously resigned to discomfort.
As much as I stress the importance of medical treatment, I put equal weight on patient education. I can’t overstate how empowering it is to understand your condition. Knowing what aggravates your symptoms and how to manage your environment is pivotal. It’s your daily life, and small, informed decisions can greatly alleviate DES symptoms.
Transitioning to the next phase of living with this condition, it’s crucial to note that life with Dry Eye Syndrome isn’t static. It’s an ongoing process, where you adapt, learn, and find new ways to maintain a high quality of life, sometimes with the help of a strong support system and ample resources.
Voice of Experience: Living with Dry Eye Syndrome
Real stories from individuals with Dry Eye Syndrome (DES) can be far more illuminating than statistics alone. Hearing about the daily challenges and triumphs offers a sense of community and understanding to those affected. I want to share with you narratives that others have generously contributed, providing insight into the day-to-day management of this condition.
Many have found that simple changes in their environment and daily routines can significantly relieve DES symptoms. For instance, frequent breaks during screen time, using a humidifier, and wearing protective eyewear can make a world of difference. It’s crucial to realize that such modifications are not just a one-off fix but part of a continuous approach to maintaining eye health.
Support systems are invaluable. From family and friends to patient advocacy groups, the exchange of knowledge and experiences plays an essential role in managing DES. There is comfort in knowing you are not alone in this and that others understand the reality of your experience. These channels offer both emotional solidarity and practical advice.
Looking to the future, we can anticipate ongoing advancements in DES research, bringing new treatments and understanding to light. Patient-centered care and increased awareness among healthcare providers are gaining momentum, which is great news for those within the DES community. On top of that, the commitment to nurturing patient advocacy ensures that the collective voice of those with DES is both heard and heeded.

