
If you’ve ever felt like your eyes are persistently dry, scratchy, or even watery, you might be grappling with Dry Eye Syndrome (DES). It’s a condition that’s more widespread than many realize, affecting millions globally. And I’m going to outline what it really is.
Dry Eye Syndrome isn’t just about a fleeting sense of discomfort; it can manifest through a variety of symptoms. Some people experience a burning sensation, while others might find reading or looking at a screen for long periods becomes uncomfortable. Some even see their vision fluctuate throughout the day.
This isn’t just about feeling uncomfortable. Dry Eye Syndrome can hamper daily functions, making tasks that require visual concentration quite taxing. It might come as a surprise, but DES can also affect emotional well-being, leading to frustration and stress over the persistent symptoms.
Don’t worry too much about confusing general eye irritation with DES. Many people do. But here’s the crux: proper diagnosis of Dry Eye Syndrome is a stepping stone to relief.
Meibomian Gland Dysfunction: A Hidden Culprit Behind Dry Eyes
I’m going to introduce you to something that might not be on your radar yet: the Meibomian glands. These tiny structures in your eyelids play a superstar role in keeping your eyes comfortable and lubricated. When they don’t do their job properly, due to what’s called Meibomian Gland Dysfunction (MGD), you might end up with Dry Eye Syndrome.
So how does MGD contribute to those gritty, burning sensations in your eyes? These glands secrete oil that forms the top layer of your tear film, preventing rapid evaporation of your tears. If the glands are clogged or aren’t secreting enough oil, your tear film becomes unstable, leading to dry eyes.
You might be wondering what puts you at risk for MGD. Age is a big factor, so is wearing contact lenses, and even environmental conditions can play a part. Oh, and if you love your screen time, listen up: sustained focusing on screens often leads to reduced blinking, which can exacerbate MGD.
If you’re thinking this is just another inconvenient condition you can shrug off, think again. The relationship between your lifestyle choices and MGD is significant. From dietary habits to daily screen time, the choices you make can impact your Meibomian glands and consequently, your eye comfort.
A key part of tackling MGD is understanding your symptoms and the impact those symptoms have on your eyes and overall lifestyle. With that understanding, you can work with your eye care professional to create a game plan that addresses both the symptoms and the underlying dysfunction.
Diagnosis and Evaluation: A Step Towards Relief
I’m going to walk you through what you can expect when getting a diagnosis for Dry Eye Syndrome and Meibomian Gland Dysfunction. The first step is recognizing the symptoms, which might compel you to see an eye care professional. Your eye doctor will likely conduct tests to evaluate the quality of your tears, the health of your Meibomian glands, and the overall surface of your eyes.
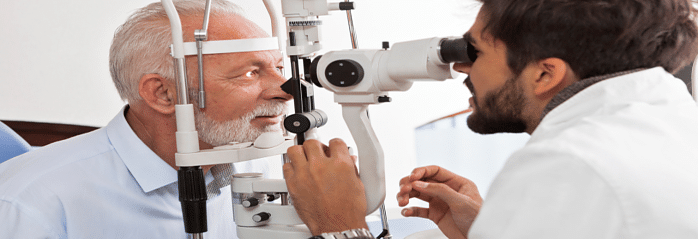
These evaluation methods aren’t something to worry about. They often include non-invasive imaging to inspect the Meibomian glands and tests like the Phenol Red test or tear breakup time. The goal is to find the root cause of your symptoms and to assess how your tear film is functioning.
Why is early detection so critical? If you want to avoid the potentially debilitating effects of chronic Dry Eye Syndrome, catching it early can prevent complications and provide a clear avenue for targeted treatment. Regular eye examinations should be part of your health checks, especially if you’re at risk or experiencing symptoms.
In my opinion, incorporating the patient’s unique experiences and symptoms into the diagnostic process is paramount. Each person’s encounter with Dry Eye Syndrome and Meibomian Gland Dysfunction is unique, and personalized care will make a tremendous difference in managing the condition.
Effective Management of Dry Eye and Meibomian Gland Dysfunction
Navigating dry eye and Meibomian Gland Dysfunction (MGD) goes beyond the occasional use of eye drops. It requires a structured approach, bringing relief and ensuring long-term eye health. You’re going to find out about treatments ranging from warm compresses to more specific medical interventions.
When it comes to home remedies, simple steps like staying hydrated, using humidifiers, and blinking exercises can provide some relief. Choose something that resonates with you and fits into your daily routine. For those needing more support, various prescription treatments, such as topical antibiotics or anti-inflammatory eye drops, can help tackle the root causes of inflammation.
Don’t worry too much about being confined to one treatment option. You can always adjust your approach down the road. If symptoms persist or worsen, advanced in-office procedures are available, including thermal pulsation treatment, which can be quite effective in unclogging the Meibomian glands.
The future of dry eye and MGD management is promising, with ongoing research opening doors to new therapies every day. There’s a lot of opportunity in staying abreast of these developments, as emerging treatments may offer even greater relief.
Most importantly, I’m here to help you understand that proactive and regular eye care can prevent the escalation of symptoms. Your first attempt doesn’t need to be your last. Just don’t focus too much on perfection; managing dry eye and MGD is an ongoing process, and staying informed is a battle half won.
